CURRENT LOCATION
5108 Mullen Road NW
Edmonton, AB
T6R0S9
PH- (587) 409-4495
Terwillegar – Edmonton
5108 Mullen Road NW
Edmonton, AB
T6R0S9
Call: (587) 409-4495
E-mail: info@mssphysio.com
Windermere – Edmonton
1301 Windermere Way SW
Edmonton AB
T6W 2P3
Call: (587) 400-1113
E-mail: windermere@mssphysio.com
Terwillegar – Edmonton
5108 Mullen Road NW
Edmonton, AB
T6R0S9
Call: (587) 409-4495
E-mail: info@mssphysio.com
Windermere – Edmonton
1301 Windermere Way SW
Edmonton AB
T6W 2P3
Call: (587) 400-1113
E-mail: windermere@mssphysio.com
Our physiotherapists and massage therapists are fully qualified to diagnose and treat pain, injuries, and chronic conditions in the Edmonton Physical therapy clinic. Any one of our therapists is happy to help you recover 100%!
Registered Physiotherapists
Occupational
Therapist
Graham Ciciarelli
Occupational Therapist
Registered Massage Therapist
Vivien Paderan
Registered Massage Therapist
Manual Lymphatic Drainage Massage Therapist
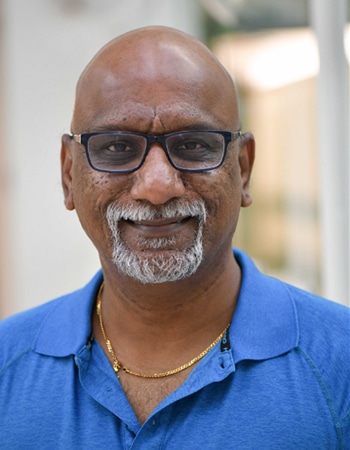
Prakash
Registered Massage therapist
Specialized in Lymphatic massage
Registered Provisional Psychologist
Acupuncturist
Certified Physiotherapy Assistants
Kersee Johnson
Physiotherapy Assistant
Murk Puri
Physiotherapy Assistant
Monique Leblanc
Physiotherapy Assistant
Office Staff
Mon 8AM – 8PM
Tues 8AM – 8PM
Wed 8AM – 8PM
Thurs 8AM – 8PM
Fri 8AM – 8PM
Sat 9AM – 2PM
We are happy to provide direct billing for our Edmonton Physiotherapy and Massage Therapy patients. We understand that this can make the process easier for patients looking for Physical therapy near me. Please contact our office at (587) 409-4495 with your insurance information and we can assist in obtaining the details of your specific plan and payment options.
Momentum Physiotherapy Edmonton
We Offer A Unique Approach To Physical Therapy!
How We Can Help Your Aches & Pains
Orthopedic & Sports Therapy
Pelvic Floor Therapy
Vestibular Therapy
Massage Therapy
Car Accident Physiotherapy
Psychological Services
EDMONTON PHYSIOTHERAPY CLINIC -
RECOVER FASTER, PERFORM BETTER, STAY IN THE GAME
We Help Patients With a Varity Of Conditions.
Back Pain
Neck Pain
Shoulder Pain
Hip Pain
Knee Pain
Foot Pain

Integrated Wellness and Physiotherapy Clinic in Edmonton
Momentum is a multidisciplinary community clinic that stands out from conventional physiotherapy clinics in Edmonton. We boast a team of skilled therapists and exercise experts who collaborate closely with each other, the community, and our clients.
Our treatment approach is rooted in scientific evidence and is tailored to meet individual needs. Our unique open-space concept aids in providing a customized program that aligns with your capabilities, lifestyle, and aspirations.
Seeking online treatment or rehabilitation based on scientific evidence? We provide TeleRehab and at-home physiotherapy options, allowing you to receive care in the comfort of your own home.
GREAT PHYSIO SOLUTIONS FOR ALL YOUR SPORTS INJURIES.
MOMENTUM PHYSIOTHERAPY CLINIC FOR ACTIVE LIFESTYLE.

Our Service Footprint
Easily tap into our customized physiotherapy services crafted to cater to your unique requirements.
- Oliver
- Terwillegar
- Windermere
- Downtown Core
- Northwest Edmonton
- Glenora
- Westmount
- Inglewood
- Highlands
- South Edmonton Common
- Beverly
- Clareview